A left ventricular assist device (LVAD) or simply a ventricular assist device, is a mechanical electronic device which is used as a pump for the heart. Mostly, LVAD is implanted when the heart's condition has been deteriorating, that can potentially lead to heart failure. The LVAD is surgically implanted, which is aids in lifting the left ventricle (main pumping chamber of the heart) pump blood to the rest of the body.
However, don't confuse LVAD for an artificial heart. The artificial heart replaces the failing heart whereas the LVAD instead of replacing the heart, assists it does its job. LVAD is a very good medical option for the patients who are too weak to get open heart surgery to treat heart disease or are in a long queue to get a heart transplant. Sometimes, a permanent LVAD is used for patients who are terminally ill and now their condition may not allow them to get extensive and complicated surgery such as a heart transplant. This treatment is also called destination therapy.
When a patient receives an LVAD while he is waiting for a heart transplant, it’s called a bridge to transplant. The patient’s LVAD may provisionally aid in pumping blood till the time a heart donor becomes available for a heart transplant.
In a situation where the patient may be declared ineligible for a heart transplant, an LVAD implant becomes the permanent solution. This is called destination therapy which has been becoming more common since the time LVAD's benefits are having a huge impact on lives on people who had a diseased heart before LVAD surgery.
When an LVAD is implanted for temporary heart failure, the type of implant is called bridge to recovery. In some cases which are rare, a heart may recover its strength after being given time to relax by an LVAD implant for the time being.
Doctors often resort to using an artificial heart to replace the ventricle's function in the heart. Individuals with severe heart failure might benefit from this gadget since it aids blood circulation throughout the body. These devices are used not just as a bridge to a heart transplant but also by many patients instead of a transplant altogether.

Unfortunately, heart failure is a progressive illness that, if left untreated, may lead to the latter stages of the disease and ultimately death. Patients with end-stage heart failure have a wide range of unpleasant symptoms, including chronic shortness of breath and fatigue, fluid retention in the lungs and belly, respiratory failure, and severe swelling of the lower limbs.
Patients needing a heart transplant often utilize the Medtronic HVAD System, a ventricular assist device. Bridge-to-transplantation describes this use. Patients with end-stage heart failure who are either not candidates for a heart transplant or whose condition prevents them from receiving one and whose complaints cannot be controlled by medicine may also benefit from the Medtronic HVAD System.
Destination treatment is used for this purpose and may enhance a patient's health and lengthen their life. The Medtronic HVAD System benefits the heart by delivering extra blood flow and helping the weak left ventricle.
The Medtronic HVAD System consists of a pump that is placed in the pericardial space, a controller that regulates the pump's speed and operation, a tube that is placed in the heart to empty the blood, and then a tube that is placed in the aorta to carry the blood away from the body.
The pump is implanted under the patient's skin, and a flexible line connects it to the controller, which stays outside the body. Batteries or an AC adapter may be used to power the controller.
Now that it has received FDA approval, the HeartMate 3 LVAD may be used by patients with advanced heart failure who are not good transplant prospects. Those patients will have to carry their pumps around with them forever. Strong long-term evidence backs up significant advances, including a pump that aims to decrease problems while increasing the survival of patients.
The Heartmate 3 LVAD has reimagined how blood is pumped via a cardiac pump and set a new benchmark for compactness and efficiency in the field. The HeartMate 3 pump uses Full MagLev Flow Technology, which improves flow while also reducing the damage experienced by the blood as it is pumped through the device.
Clinical results from the MOMENTUM 3 study supported the approval of the HeartMate 3 system in the United States. The HeartMate 3 research found an unprecedented two-year survival rate of 83% for individuals using the device.
Blood clots in the pumps were uncommon, with just 1% of patients experiencing a suspected thrombosis after two years. In addition, the two-year stroke rate for the continuous-flow LVAD in the trial was the lowest.. ever reported.
Patients with intermediate to severe stages of heart failure may benefit from either temporary or permanent circulatory assistance provided by the HeartMate IITM Left Ventricular Assist Device (LVAD). This compact and silent pump has a simple design, consisting of just one working element, and can provide blood flow comparable to that of a functional heart.
Suppose the pump develops thrombosis, malfunctions, or becomes infected. In that case, the HM2 LVAD may need to be replaced, given both a description of a unique minimally invasive procedure developed for exchanging HM2 with the latest generation of intrapericardial pumps known as HVAD or HM3 as well as our clinical experience using this technique.
All patients who had a device exchange at our hospital from a HeartMate 2 to a HeartMate 3 were evaluated retrospectively. Survival rate at six months was considered the primary outcome, whereas surgical outcomes and discharge disposition were investigated in a supplementary study.
The Fisher's exact test and the Mann-Whitney U test were used to compare the baseline parameters and the clinical data.
If you are a patient who is seeking to get receive an LVAD implant, you may be having heart disease or progressive heart failure which can not be treated. The cardiologists implant an LVAD on the heart which is sick, but not too sick overall since that would make the LVAD implant surgery a little risky.

To check if the heart is diseased enough, and if the rest of the body is in a decent position to receive an LVAD implant, the cardiologists might run a number of objective tests.The result of these objective tests will help the cardiologist and his team evaluate if getting an LVAD implant is a good fit for you, your heart and the body.
However, LVAD may not be a good choice of surgical treatment for heart disease if you have:
For patients suffering from advanced heart failure, getting an LVAD implant may bring out benefits which are more than expected.
Some of the benefits of LVAD include:
An LVAD consists of:
Implanting an LVAD in the heart may take from four to six hours to complete. LVAD is a device which can pump blood just like like the heart. One of the ends of the LVAD is attached to the left ventricle of the heart which is the part or chamber of the heart responsible for pumping blood out of the lungs through the other parts of the body. The second end of the LVAD is attached to the aorta, which is the body's main and longest artery. The heart pumps blood from the left ventricle into the aorta through the aortic valve. A tube passes through the skin reaching to the device. The exterior of the tube is coated in a special material which helps in healing, allowing the regrowth of the skin. The pump and all its connections are implanted when the cardiologist makes incisions to conduct open-heart surgery.
The other surgery equipments consist of a computer controller, a power pack, and a reserve power pack but they function outside the body and are not planted into the interior. Despite the small size of the LVAD, it is capable enough to pump blood every minute in order to curb the heart failure/disease symptoms. The cardiologist will regulate the LVAD pump so that there's an adequate flux of the blood to meet body needs. A connection between the driveline and the pump is made. The cable that connects the pump to the controller is fed through a small incision in your abdomen.
Artificial heart transplantation is a complex procedure that replaces the ventricles of the heart with an artificial one. CureIndia helps you choose the best doctor for your artificial heart transplantation in India. The surgeons associated with CureIndia are highly experienced and specialised in their fields, providing the best possible treatment with visible results. Let's hear from some of the leading doctors for artificial heart transplantation in India:
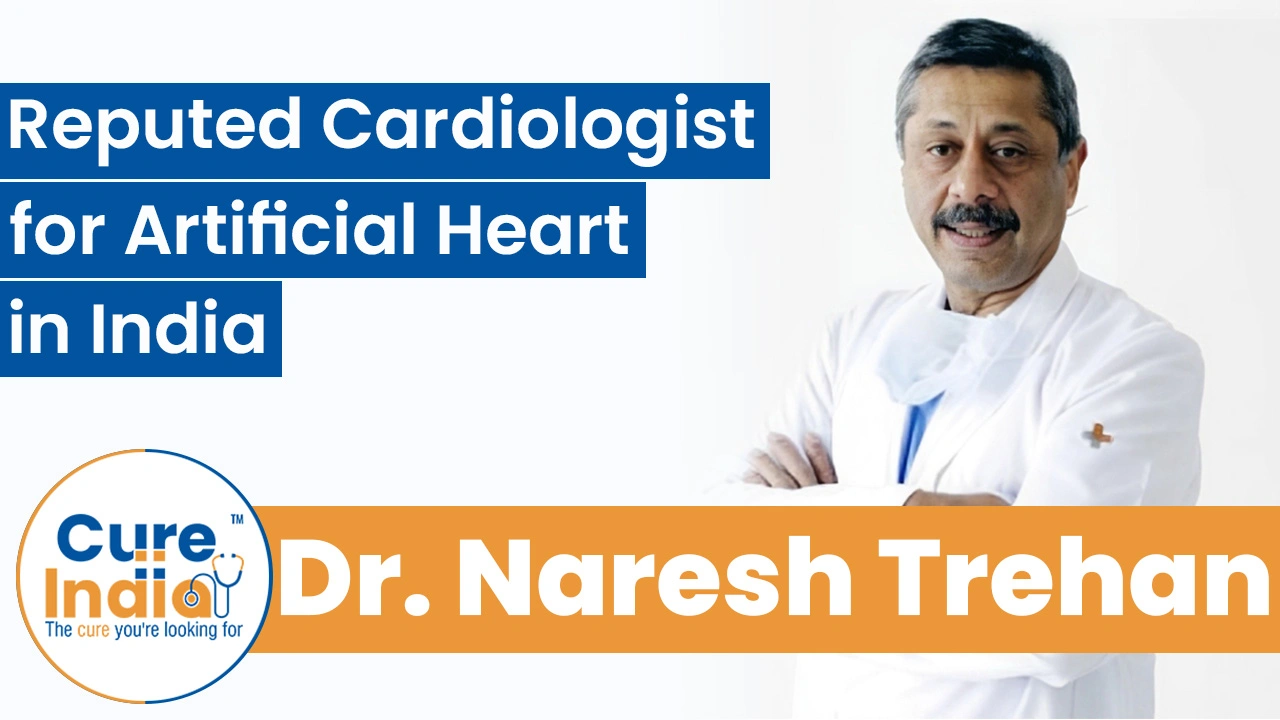
Dr. Naresh Trehan is one of India’s most reputed cardiac surgeons, with nearly 52 years of experience in cardiothoracic and cardiovascular surgery. As a surgeon specialising in advanced cardiac care, he has performed over 48,000 open-heart surgeries, including ones involving artificial heart devices and mechanical circulatory support systems. Dr. Trehan is known for his expertise in heart transplantation, aortic valve replacement, and minimally invasive cardiac surgery.
Dr. T. S. Kler is a top-rated cardiac surgeon in India with over 30 years of experience in performing cardiac procedures such as artificial heart transplants. As chairman of heart & vascular Surgery at BLK-Max Hospital, he has performed thousands of advanced cardiac surgeries, including those involving artificial heart devices and mechanical circulatory support systems.
Dr. Z S Meharwal is a leading cardiac surgeon in India, with over 30 years of experience in cardiothoracic surgery and heart transplantation. A founding member of the Fortis Escorts Heart Institute, he has performed more than 30,000 complex cardiac procedures till date, including advanced surgeries involving artificial heart transplants.
Dr. Kuldeep Arora is a senior consultant cardiologist at Artemis Hospital, Gurgaon, with over 16 years of expertise in interventional cardiology. Till date, he has successfully performed more than 12,000 therapeutic cardiac procedures, including artificial heart transplantation, coronary angioplasties, permanent pacemaker implantations, AICD and biventricular pacemaker placements, and atrial septal defect device closures.
The cost of artificial heart surgery in India is around $65,000, and can reach up to $115,000, depending on the device used and the hospital’s infrastructure. The total expense varies based on pre-operative evaluations, ICU stay, post-operative care, and the patient’s condition, which might require additional medical support. Compared with other heart procedures like bypass or valve surgery, which cost far less, artificial heart implantation remains one of the most advanced and expensive cardiac treatments available in India.
| Treatment Name | Cost in India | Stay in India |
|---|---|---|
| Artificial Heart Transplant in India | $65,000 - $115,500 | 2 Months |
Left ventricular assist devices have improved survival for people with end-stage heart failure. Modern studies consistently show that LVAD implantation roughly doubles the one-year survival rate compared with advanced medical therapy alone.
In many major heart-failure centers, one-year survival after LVAD implantation is commonly reported in the 75-85% range, though outcomes vary based on patient health, device type, and center expertise. Beyond survival, LVADs often improve quality of life, exercise capacity, and symptom control for patients who are not immediate candidates for heart transplantation.