An estimated 80 million people worldwide suffer from thalassaemia, making it a global health concern. Unfortunately, there are still many countries that lack awareness and understanding of thalassemia and its treatment. While some countries face challenges related to healthcare infrastructure and specialised resources, others, like the UK and the USA, offer advanced treatment options, but at a higher cost, making them less accessible to patients with financial limitations.
India, on the other hand, has become a top location for thalassaemia treatment due to its combination of low costs, modern medical facilities, and highly qualified experts. India places a strong emphasis on early diagnosis and efficient disease management in light of the difficulties faced by those who have thalassaemia. Because of this, the nation is becoming more and more known for offering both domestic and international patients high-quality and reasonably priced healthcare.
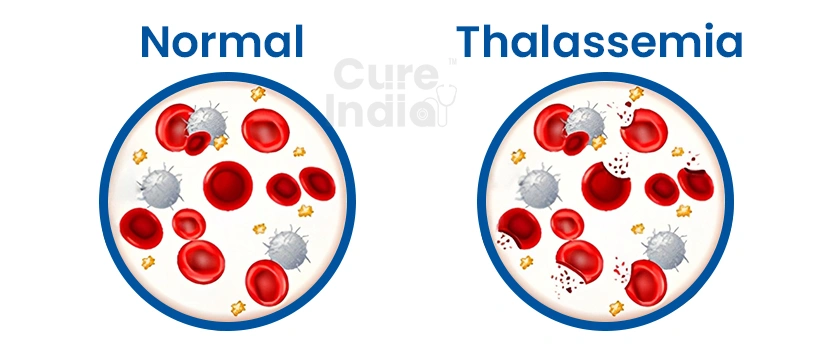
Thalassemia is an inherited blood disorder that impacts your body’s crucial protein needed for making haemoglobin and red blood cells. Since haemoglobin enables your red blood cells to carry oxygen throughout your body, supplying the other cells with nutrients, the deficiency results in reduced oxygen transport throughout the body, causing symptoms such as anemia, fatigue, pale skin, and shortness of breath. When you get affected by thalassemia your body reduces its hemoglobin production depriving your body’s cells of the oxygen, they require to create energy and thrive. This can further lead to severe complications like bone deformities, growth retardation, and organ damage.
While there are thalassemia major vs minor types that require different treatment approaches, their symptoms tend to be anemia-like symptoms that range from mild to severe. Treatment options are mostly determined based on medical history, age and severity of the condition. This treatment page will aware you on everything you need to know about getting thalassemia treatment in India.
There are different thalassemia types based on which globin genes alpha or beta are affected. The severity of the condition depends on how many gene mutations are inherited and from which parent:
Since you tend to inherit four genes, two from each parent, that make alpha globin protein chains, where even a single defective gene can result in alpha thalassemia. Alpha thalassemia occurs when one or more of the four genes that make alpha globin protein chains are defective. The severity of the condition you experience depends on the number of defective genes:
This condition mainly happens when you inherit two beta-globin genes, one from each parent. While the severity of the condition depends on the number of genes that are defected and the location of the defect, here’s how you might feel for each condition:
Thalassemia symptoms vary depending on the type and severity of the condition. These symptoms play a key role in determining the most appropriate treatment plan. The symptoms are classified into:
Some patients, especially those with alpha thalassemia minima or beta thalassemia minor, may not exhibit any obvious symptoms. These cases often go un-diagnosed unless detected through routine blood tests. However, mild fatigue or persistent tiredness can sometimes be present.
In cases of thalassemia intermedia or mild forms of hemoglobin H disease, the symptoms include:
Severe thalassemia, such as beta thalassemia major or severe haemoglobin H disease, can cause:
Before going for thalassemia treatment, you must undergo some evaluation and blood tests to diagnose the disorder properly. The tests required to diagnose thalassemia may vary depending on the suspected type of thalassemia and the patient’s individual symptoms and medical history. Here is a list of tests that are used to diagnose thalassemia:
This test measures the levels of red blood cells, white blood cells, hemoglobin, and platelets. Thalassemia is indicated by:
This test identifies and quantifies the different types of haemoglobin in the blood. Patients with thalassemia often have abnormal forms or imbalanced levels of haemoglobin, which helps differentiate between thalassemia types.
Iron tests, including serum ferritin, iron, and total iron-binding capacity help distinguish thalassemia from iron-deficiency anaemia. While both conditions cause low haemoglobin, iron levels are normal or elevated in thalassemia.
Genetic testing detects mutations in the globin genes responsible for thalassemia. It confirms the diagnosis and identifies carriers, even in asymptomatic patients. It is particularly useful for family screening and planning.
The prenatal diagnostic methods include Chorionic Villus Sampling and Amniocentesis. This test involves taking a sample of the placenta or amniotic fluid, respectively, for genetic testing, and is performed during pregnancy to determine if a foetus has thalassemia.
However, the moment you are diagnosed with thalassemia, try to consult a healthcare specialist for an accurate treatment plan to get an effective thalassemia treatment.

Whatever your causes of thalassemia might be, it’s important to avoid putting yourself in those situations during and after the diagnosis and treatment. However, once you are evaluated and thoroughly checked, depending on your health condition and the severity of the disorder, your doctor might suggest one of the following options for thalassemia treatment in India:
Folic acid supports the production of healthy red blood cells. Your doctor can recommend these supplements, especially in the early stages of treatment or for patients with mild forms of thalassemia.
Regular blood transfusions are crucial for moderate to severe thalassemia treatment. They help maintain healthy haemoglobin levels and ensure the body receives adequate oxygen. Depending on the severity, transfusions might be needed every few weeks.
Frequent transfusions can lead to iron overload, which can damage vital organs such as the heart and liver. Iron chelation therapy removes excess iron from the body using medications such as Deferasirox and Deferoxamine.
In cases where the spleen becomes enlarged and starts destroying red blood cells excessively, a splenectomy is advised. This surgery helps improve the effectiveness of blood transfusions and reduces the need for them.
A bone marrow transplant is currently the only curative and most effective thalassemia treatment method. Here, the patient’s bone marrow is replaced with healthy stem cells from a compatible donor, ideally a sibling. While highly effective, it is recommended in severe cases and requires a suitable donor match and access to advanced medical facilities for a successful transplant.
Thalassemia patients need regular monitoring for complications like heart problems due to iron overload, bone deformities, and infections.
Recovery after thalassemia treatment in India varies depending on the severity of the condition and the type of treatment received. While milder forms can be effectively managed with routine care, severe cases require lifelong monitoring and support. Although stem cell transplants can be a potential cure for severe forms, but finding a compatible donor can be difficult. After treatment, patients are provided with a personalised recovery plan that includes medication, dietary and lifestyle adjustments, and regular medical follow-ups. These follow-ups involve complete blood counts, iron studies, and annual tests for heart and liver function, as well as screenings for viral infections. For patients who have undergone transfusions, yearly assessments for iron overload such as MRI or FerriScan are necessary to prevent long-term organ damage. Adhering strictly to your doctor’s recommendations and attending regular check-ups help maintain stability, prevent complications and improve the overall quality of life after treatment.
When it comes to thalassemia, timely intervention, consistent monitoring, and access to advanced therapies can make all the difference. Our leading hematologists and BMT experts combine their decades of experience with advanced treatments to manage thalassemia. Here is our list of top thalassemia treatment doctors in India:
Dr. Gaurav Dixit is a leading doctor for thalassemia treatment in India with specialised expertise in treating benign hematological disorders, including thalassemia, sickle-cell disease, and aplastic anemia. He has been involved in over 1,000 bone marrow transplant procedures and over the years has built experience treating blood disorders requiring transplant and long-term management.
Dr. Rahul Bhargava is a leading hematologist and bone-marrow transplant expert in India. Till now, he has performed well over 1,000 BMT procedures, including transplants for thalassemia major and other complex blood disorders. He has also played an important role in setting up low-cost BMT and transplant centres across India to make high-level hematological care accessible and affordable to everyone.

Dr. Dharma Choudhary is an expert thalassemia surgeon in India. He has over 20 years of experience in this field and is currently the chairman of hemato-oncology and bone marrow transplant at BLK Max Super Speciality Hospital. His areas of specialisation include bone marrow transplantation and non-malignant blood disorders such as thalassemia and aplastic anemia.
Dr. Pawan Kumar Singh is an advanced thalassemia treatment doctor in India with more than 21 years of experience in haemato oncology and bone marrow transplants. Till now he has performed hundreds of BMTs, including complex transplants for thalassemia, sickle-cell disease, and other blood disorders for both pediatric and adult patients, including matched sibling, haploidentical, and unrelated donor transplants.
While BMT can be an expensive option for thalassemia treatment in countries like USA, UK, Africa and Thailand, in India the cost ranges from $20,400 to $47,600, depending on the hospital or private clinic, transplant procedure, hospital stay, medication regimen and associated care. Furthermore, India offers a success rate of 60% - 70% in thalassemia treatment, offering the best international alternative at a cheaper price than countries like Africa, the UK, the USA and Thailand. India’s affordability, success rate and well-credited hospitals make it a popular choice for patients of African countries, like Ghana, Ethiopia, Congo, and Kenya.
| Treatment Name | Cost in India | Stay in India |
|---|---|---|
| Thalassemia Surgery in India | $20,000 - $40,000 | 2 - 3 Months |